The Economics of Occupational Health: How WorkCare’s Injury Care Telehealth Triage Model Reduces Costs, Risk, and Lost Time
Workplace injuries cost more than they should because care starts in the wrong place. This white paper explains how WorkCare’s Injury Care telehealth triage model reduces claims, cuts recordables, and improves employee outcomes.
Executive Summary
Workplace injuries remain one of the most persistent and expensive operational challenges for employers. While some employers invest in preventive approaches, others assume injuries are a cost of doing business, feeling that they have little control over how care unfolds once an employee reports an incident. This is an old-school assumption that contributes to higher costs and poorer health outcomes. The majority of work-related injuries are not serious and can be safely managed at onset, before they get into the workers’ compensation system.
WorkCare’s Injury Care 24/7 telehealth triage delivery model is a proven way for employers to change the financial equation and ensure quality care. By giving employees immediate access to WorkCare’s occupational health clinicians, companies prevent unnecessary clinic and hospital emergency room visits, reduce OSHA-recordable rates, and effectively manage safe work during recovery – eliminating delays that drive up costs.

This white paper explores what drives these outcomes and why the Injury Care telehealth triage model is one of the most effective, measurable strategies to reduce workers’ compensation costs while improving employee outcomes.
I. The Cost Problem Employers Can’t Ignore
Large employers invest heavily in safety teams, risk managers, and operational leaders to control exposure and respond quickly when injuries happen. These professionals understand the financial impact of delayed care, unnecessary ER visits, and treatment decisions that escalate what could have been a simple first-aid case. What’s often overlooked is how much of this cost is tied not to the injury itself, but to where and how employees receive care in the first minutes after an incident.
Most organizations do everything they can to avoid the ER unless it’s a true emergency; the costs and wait times speak for themselves. But even routine clinic visits add avoidable expense when clinicians don’t understand the work environment, the job tasks involved, or the employer’s return-to-work expectations. That lack of context drives overtreatment, unnecessary time off, and unnecessary claims. Employers don’t necessarily need a board-certified occupational medicine physician for every case. They need a responsive provider who understands their industry and communicates with them in real time.
This gap shows up in predictable ways. An employee strains his back, cuts her hand, or twists a knee. Without clear direction, the employee walks into an ER, urgent care clinic, or their personal doctor’s office. Providers unfamiliar with the physical demands of the job may order imaging, prescribe rest days, and classify the injury based on general practice medical standards instead of occupational health protocols. The result is predictable:
- A minor injury becomes a recordable case.
- Lost time increases because an external provider takes the conservative route.
- Cases become claims that could have been resolved with guided self-care and safe return to work during recovery.
These decisions ripple through operations. They affect staffing, overtime, compliance reporting, insurance premiums, and employee morale. The connection between costly operational consequences and the lack of an early clinical gatekeeper is often overlooked by leadership. In truth, workplace injuries cost more than they should when employers allow care to start in the wrong place and escalate from there.
Occupationally oriented telehealth triage and telemedicine services are a good place to start because they provide rapid assessment, right-sized care, and immediate communication – and at a fraction of the cost of an offsite clinic or ER visit. For most employers, provider responsiveness and alignment with real job demands matter far more than academic and medical credentials alone.
II. The Simple Shift That Changes Everything
Experience shows that the faster an employee receives care for a non-emergent injury, the lower the overall cost. With WorkCare’s Injury Care and telehealth triage model, employees are encouraged to immediately report injuries, including aches and pains that they may assume will get better on their own. They are connected with an occupational health clinician, not a general practitioner, not a supervisor making judgment calls, and not a local provider who is unfamiliar with OSHA rules or modified duty options.
That single shift produces these downstream benefits:
Employees get immediate answers. No waiting rooms. No delays. No guesswork. Clinicians help employees understand the injury, what to do next, and determine whether they should see a local provider for further evaluation and potential treatment.
Supervisors are removed from medical decision-making. They no longer have to evaluate severity or guess whether an employee should receive first aid onsite or be sent offsite for care.
Care becomes consistent across every work location. One clinical standard. One triage process. One documentation model across a business enterprise.
Recordability decisions become defensible. Clinicians trained in OSHA reportability and recordability determinations document every step, giving safety leaders clarity and legal protection.
Self-care becomes the norm, not the exception. Employees become comfortable with self-administered first aid when care guidance is clear and based on established clinical protocols. That directly reduces costs.
III. The ROI Story Backed by Real Outcomes
The most compelling proof of this model isn’t theoretical, it’s the actual outcomes employers see once they transition to a clinically managed injury response system.
Check out these real-life examples of ROI from WorkCare Injury Care Clients:
- A retailer reduced its annual costs by $510,000
Program cost: $60,500
ROI: 8.4:1
Minor injuries were handled through clinician-guided self-care, preventing unnecessary claims.
- A construction firm saved $1.5 million in the first year
Program cost: $275,000
ROI: 5.5:1
This is a workforce with high physical demands and significant injury exposure. A centralized triage model cut claim costs by 12 percent in year one.
- An engineering company reduced incurred claims by $186,000
Program cost: $39,000
ROI: 4.8:1
Early intervention avoided prolonged medical care and unnecessary lost time.
Individually, these results are impressive. Together, they point to a larger truth:
The financial value of a triage-first Injury Care model is proven, repeatable, and scalable across industries.
IV. What Drives These Results: The Operational Mechanics
To understand why the ROI is so consistent, you have to look at the operational realities of injury response.
When employees receive immediate clinical triage:
1. They avoid unnecessary medical treatment
Key Metrics by Industry
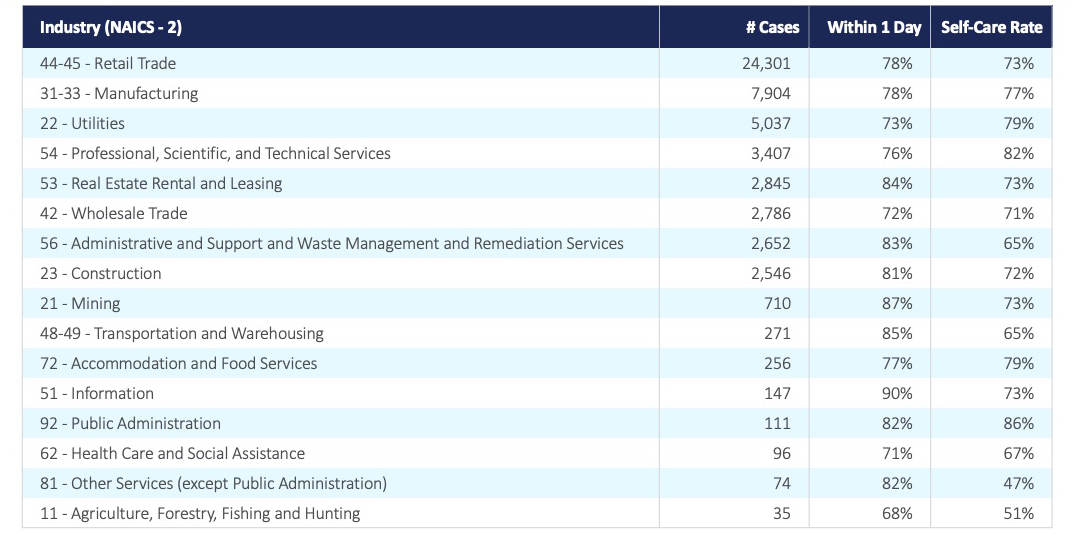
A significant percentage of workplace injuries can be safely treated with clinician-guided self-care. Without guidance, minor cases often escalate from non-recordable first aid to OSHA-recordable incidents and workers’ compensation claims.
Before implementing the Injury Care model, industry data show that self-care typically occurs about 50 percent of the time. With WorkCare, the self-care rate increases 68-80 percent, depending on the industry sector and the company’s degree of commitment to immediate injury reporting and early medical intervention.
2. Claims close faster and cost less
A significant percentage of workplace injuries can be safely treated with clinician-guided self-care. Without guidance, minor cases often escalate from non-recordable first aid to OSHA-recordable incidents and workers’ compensation claims.
WorkCare clients show dramatic reductions in the severity and duration of claims. Examples:
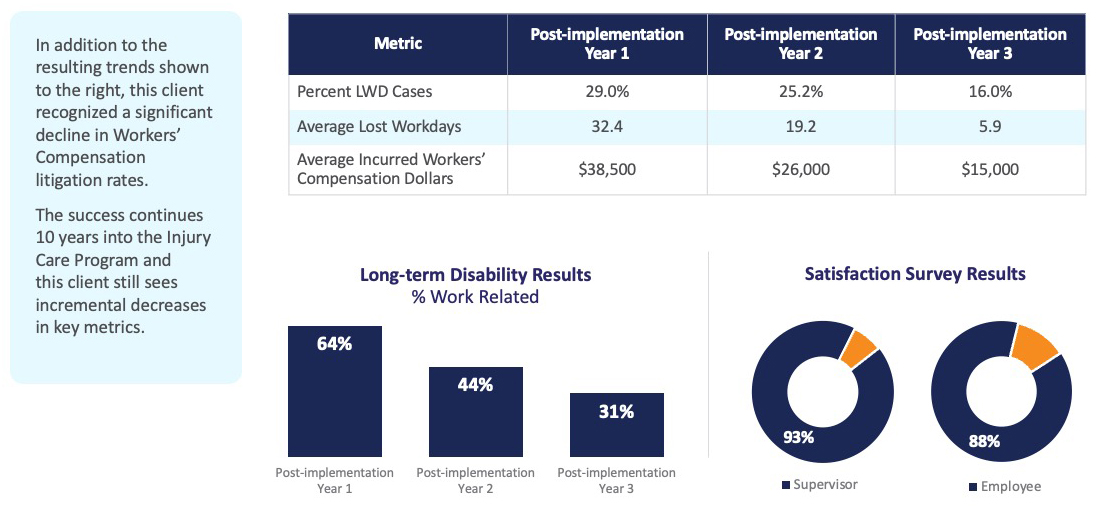
- Three years post-implementation, a large utilities client reduced lost workdays from 32.4 to 5.9 across several geographically dispersed locations:
Client Results: Large Utilities Company
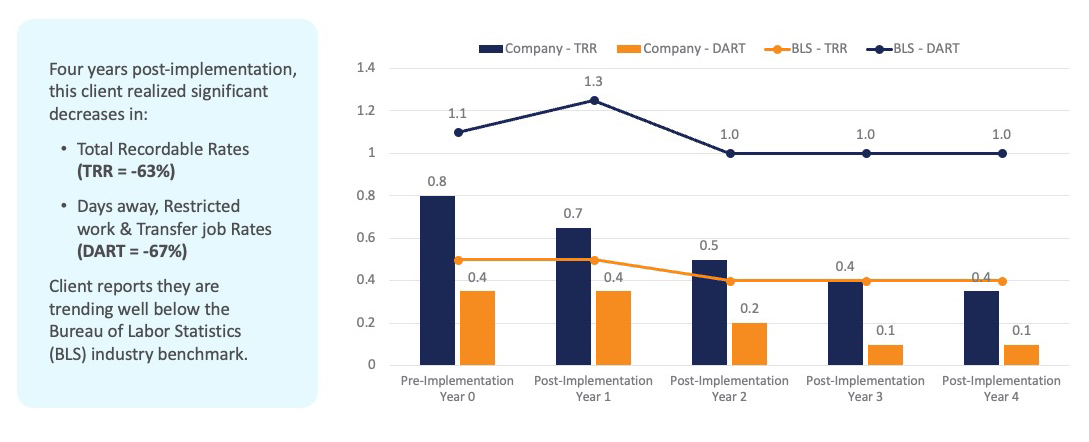
- Four years post-implementation, a professional services client reduced its total recordable incident rate by 63 percent and its DART rate by 67 percent, outperforming national benchmarks:
Client Results: Large Professional Services Company
This is why the financial impacts are so dramatic. Employers are replacing a fragmented, reactive model with a unified, clinically led process that curtails unnecessary escalation.
3. OSHA recordability becomes precise and consistent
Clinicians trained in OSHA standards make decisions that reflect each injury’s true nature — no assumptions or variability among supervisors.
4. Documentation becomes audit-ready
Every call, decision, and recommendation is recorded and defensible.
5. Engagement increases because the process is simple
When employees know who to contact and what happens next, compliance improves. That’s why satisfaction scores are so high at this large utilities company:
- 88 percent employee satisfaction
- 93 percent supervisor satisfaction
A streamlined, clinically led process produces predictable results because it replaces guesswork with expert decision-making.
V. Industry Trends and the Shift Toward Early Clinical Intervention
Across industries—from retail to utilities, manufacturing to professional services—injury patterns differ, but the underlying problem is the same: injuries escalate when early intervention is not part of the equation.
WorkCare’s cross-industry data highlight two key trends:
1. Industries with high physical demands benefit the most
Construction, utilities, manufacturing, and warehousing see immediate gains because minor musculoskeletal injuries are common — and easily resolved when handled quickly.
2. Companies outperform Bureau of Labor Statistics benchmarks once triage is implemented
Professional services clients saw recordable rates fall far below industry norms within 2-3 years.
The trend is clear: Organizations that standardize injury response outperform those that don’t—financially, operationally, and from a compliance standpoint.
VI. Telehealth Triage as the Occupational Health Standard of Care
Telehealth triage isn’t a “nice-to-have.” It’s the only scalable, consistent, compliant way to manage injuries across multi-site or distributed environments.
Employers adopt it for three reasons:
1. Speed – Employees get immediate answers. No waiting. No uncertainty.
2. Accuracy – Clinicians trained in occupational health deliver precise decisions.
3. Consistency – Every site, every shift, every incident—managed the same way.
This matters because most safety programs focus on prevention, not response. Prevention is essential, but what happens in the first 10 minutes after an injury has far greater influence on claim costs, lost time, and recordability.
Telehealth is now the most reliable way to control that moment.
VII. Implementation is Straightforward
A telehealth-first Injury Care model isn’t disruptive. It’s a simple operational upgrade.
1. Program Setup – WorkCare aligns protocols, call flows, and reporting with your organization.
2. Go-Live – Employees receive one point of contact for injuries. Supervisors are trained on when and how to use the service.
3. Continuous Improvement – Monthly reports show trends. Case management keeps claims moving. Leadership gets visibility into what’s driving costs—and what’s reducing them.
This isn’t a complicated transformation. It’s a practical shift that immediately improves outcomes.
VIII. The Business Case for Employers
Workers’ Compensation Claim Trends
(Total incurred dollars with WorkCare)
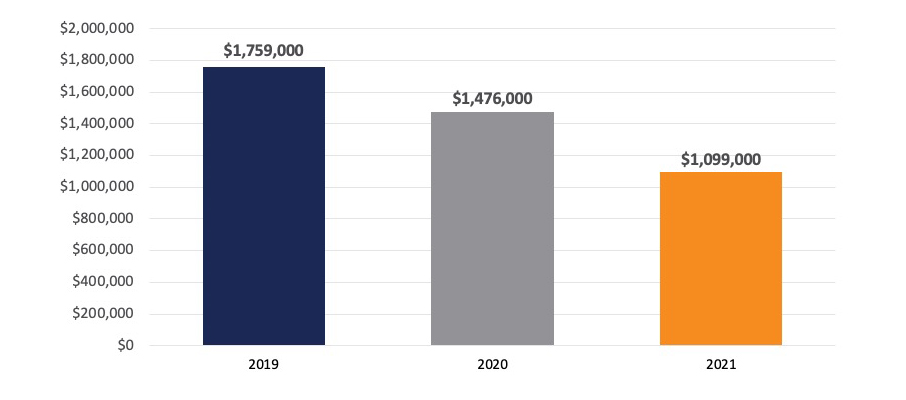
When you consolidate injury response through a clinically led model, the benefits cascade through the organization:
- Lower workers’ compensation costs
- Fewer OSHA-recordable incidents
- Reduced claim volume
- Faster case closure
- Dramatically less lost time
- Improved employee experience
- Stronger protection against audits and litigation
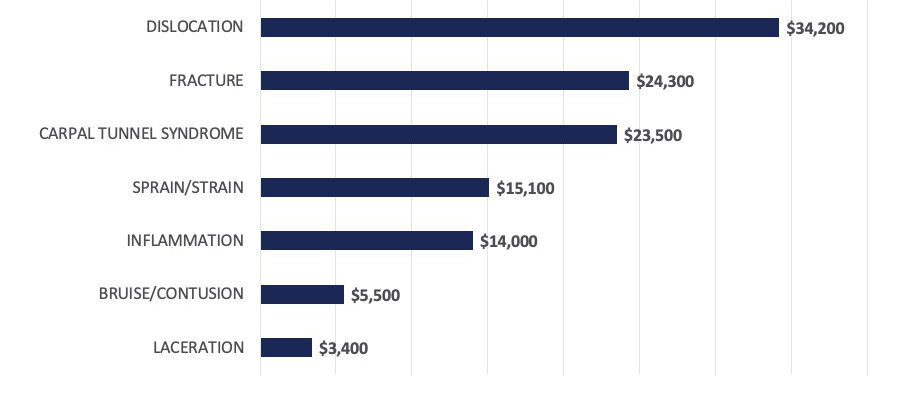
Average incurred dollars per workers’ compensation claim
(By nature of injury for 3 WorkCare clients)
Few occupational health strategies deliver this level of financial return with so little operational friction.
Conclusion
WorkCare’s Injury Care with 24/7 telehealth triage is reshaping the economics of workplace injuries by addressing the root cause of unnecessary cost: inconsistent response and delayed care. When employers give employees direct access to occupational health clinicians, they stabilize costs, reduce risk, and create a safer environment where injuries are handled responsibly and efficiently.
The results are clear. This model works. For organizations looking to strengthen both safety and financial performance, early clinical intervention isn’t just a better option, it’s the most responsible one.
To understand what this could mean for your organization, schedule a WorkCare Injury Care consultation and review your potential savings.
Let’s Work Together
Ready to take your workforce health and safety to the next level?
Contact us today to learn how WorkCare can partner with you to create a healthier, safer, and more productive workplace.
